'Policy' in the Palliative Care Context
There is a growing recognition that effective policies, laws, strategies and plans are required to promote and develop general approaches to the end of life and specifically, palliative care.
Sepúlveda et al, (2002) for example contend that “there is no doubt that there is a need to advocate worldwide for adequate policy development…...in the area of palliative care” with Stjernswärd, Foley and Ferris (2007) placing “appropriate policies” as an overarching feature of their ‘WHO Public Health Model’ that informs three secondary areas - adequate drug availability, education of health care workers and the public, and implementation of palliative care services.
In 2014, the World Health Organization (WHO) Executive Board Resolution called for the creation and strengthening of health systems that include palliative care as an integral form of treatment. This was approved by the 67th World Health Assembly (WHA).
Recent work done within the Group suggests that this Resolution has shown some early promise in generally championing palliative care, though evidence is still lacking on the impact it has had on the ground (see Carrasco, J., Inbadas, H., Whitelaw, A. and Clark, D. (2020) Early impact of the 2014 World Health Assembly Resolution on Palliative Care: a qualitative study using semi-structured interviews with key experts, Journal of Palliative Medicine,)
The Glasgow End of Life Studies Group has also developed work in a number of policy related themes:
Palliative Care Policy as Varied and Complex: A Taxonomy of Interventions
Palliative Care Policy as Varied and Complex: A Taxonomy of Interventions
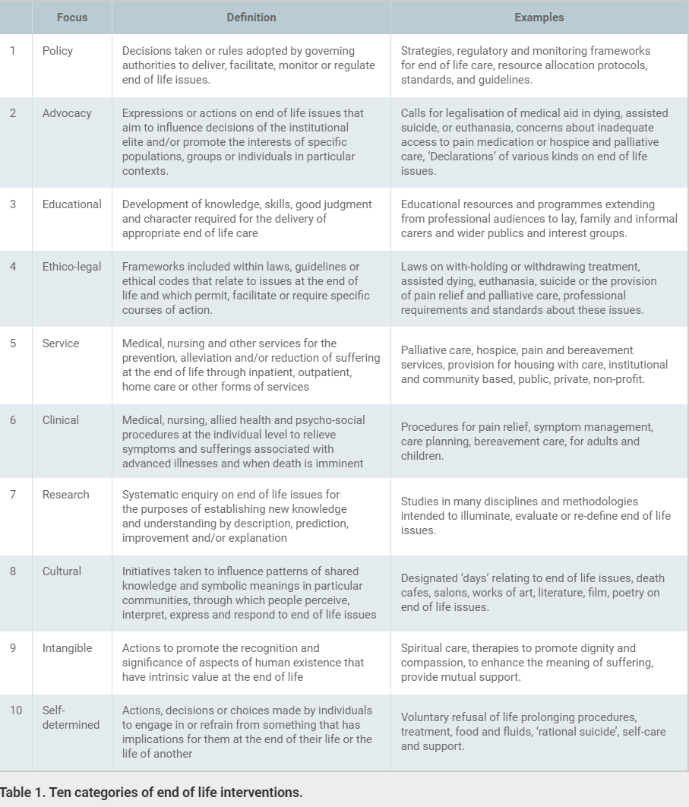
The potential breadth and complexity of the palliative care policy area is increasingly being recognised; Abel, Kellehear and Karapliagou’s (2018) for example differentiating between ‘specialist’, ‘generalist’, ‘community’ and wider ‘civic’ forms of intervention. The conceptual and practical basis of this ground was explored within a piece of work undertaken by the Group and led by Professor David Clark. 10 substantive intervention categories were identified: policy, advocacy, educational, ethico-legal service, clinical, research, cultural, self-determined. These are set out below:
Further Links
Perspectives on Global Palliative Care Policy
Perspectives on Global Palliative Care Policy
As well as individual nations pursuing the development of their own form of policy, there is a growing interest in the comparative analysis of policy in a wider global context. This work has critically highlighted the problematic nature of accepted orthodoxies on what is considered ‘high quality’ palliative care and the difficulties of simply ‘transferring’ policies and practices from one domain to another. This ground was explored within a piece of work undertaken by the Group led by Dr. Shahaduz Zaman. Drawing on subaltern and post-colonial theory, the work sought to critique and re-frame these assumptions, offering up the possibility of more pluralistic global perspectives on care for the dying.
Further Links
‘Public Health’ Policy
‘Public Health’ Policy
One specific expression of policy development within palliative care centres on the notion of the domain being seen as a ‘public health’ issue. In this context, public health informed policy suggests the need to pursue and co-ordinate a wide range of approaches and interventions – legal, clinical, educational and social. The latter theme is particularly prominent in relation to promoting community engagement and nurturing ‘compassionate communities’. Whilst various countries have adopted these principles as policy templates, work within the group has sought to critically appraise the robustness of this application, concluding that if public health is considered to have intrinsic and definable worth, the association needs to be significantly developed with much higher levels of theoretical, practical and critical engagement between the two disciplines.
Further Links
The Relevance of ‘Total Pain’ in Palliative Care Practice and Policy
The Relevance of ‘Total Pain’ in Palliative Care Practice and Policy
In 2019, Dr. Marian Krawczyk and Dr. Naomi Richards co-authored a journal article which proposed that a decades-long lack of inquiries into the concept of total pain has led to a knowledge gap and disparity in understanding between clinicians, and that a deeper understanding of total pain is a priority for the evolution of palliative care practice and policy.
The article offers a brief outline of key issues in defining total pain, considers some of the professional and system-based challenges to addressing total pain, and suggests how the substantial knowledge gap about total pain has potentially serious consequences in clinical practice and policy development. We hope this stimulates further interest and inquiry as to the relevance of total pain within the contemporary culture of palliative care.
The full article can be found here:
Krawczyk, M. and Richards, N. (2018) The relevance of ‘total pain’ in palliative care practice and policy. European Journal of Palliative Care, 25 (3); 128-130.
Find out more about our work on 'Total Pain' here.
Further Links
You can read a longer blog post about the article at the European Journal of Palliative Care website:
Case Study: Exploring the Implementation of Palliative Care Policy
Case Study: Exploring the Implementation of Palliative Care Policy
One of the best examples of considering the detailed nature of actual policy implementation within palliative care comes from work undertaken by May et al (2014) in Ireland. In 2001, this country was one of the first to develop a defined national palliative care policy.
This analysis adopted a ‘policy analysis triangle’ as a resource to review the construction, implementation and impact of the policy. Whilst noting progress, the work highlighted various difficulties in enacting policy in this emerging field. A series of issues that need addressed were identified, including navigating the complexity of the field; being conscious of the relationship between ambition and feasibility; identifying sufficient resources and the challenge of attracting these in competitive policy circumstances; and using these resources to develop workforce and general capacity
On-going Critical Lines
On-going Critical Lines
Despite the optimism often associated with calls for policy development in palliative care, there is little work that actually appraises the extent to which success is achieved on the ground and in some quarters some scepticism over the substance of such calls. As such, the Group are currently working in the following areas:
- Based on work previous work that has mapped global levels of palliative care provision [link to Clark, D., Baur, N., Clelland, D., Garralda, E., Lopez-Fidalgo, J., Connor, S. and Centeno, C. (2020) Mapping Levels of Palliative Care Development in 198 Countries: The Situation in 2017, Journal of Pain and Symptom Management, 59 (4); 794-807], the re-analysing generic data to quantify and understand the patterning of levels of policy activities across countries [David Clelland and David Clark];
- A systematic review of literature associated with palliative care policy with a view to mapping the nature of expressions (geographical spread, status, focus, intentions, stages of completion) [Sandy Whitelaw, David Clark and Anthony Bell];
- An analysis of the expression of palliative care and end of life issues in Health and Social Integration Strategies in all regions across Scotland [Anthony Bell, David Clark and Sandy Whitelaw].
End of life issues around the world: taxonomy and 'overlapping consensus'?
Professor David Clark introduces his research into end of life interventions around the world.
Common or multiple futures for end of life care around the world?
Dr Shahaduz Zaman of the University of Glasgow End of Life Studies Group introduces his paper, 'Common or multiple futures for end of life care around the world? Ideas from the ‘waiting room of history’. This article was published in Social Science & Medicine in January 2017 and is available as an open access document here.
AIIHPC Session 2 - Dr Shadhaduz Zaman
Posted by AIIHPC, January 2016

